|
|
|
Kamalpreet Singh
|
Reversal of Type 1 Diabetes on Raw Vegan Diet:
Case Report
|
|
|
Abstract
|
|
Type-1 diabetes (T1D) is an autoimmune disease in which pancreatic beta cells get destroyed, which leads to
reduced ability to produce insulin, leading to hyperglycemia. T1D may lead to irreversible health complications
such as retinal damage, chronic kidney diseases, peripheral neuropathy, systemic hypertension, and coronary
heart disease. The patient gets dependent on insulin injections for his whole life. It was believed that blood
glucose readings cannot be brought in non-diabetic range without the support of insulin injections in the case of
T1D. However, in the present case we observed the readings of blood glucose in a 13-year-old patient of T1D by
putting her on a plant-based diet. The patient was monitored for 150 days. She was successfully able to maintain
non-diabetic blood glucose readings and eliminate her insulin dependency within 14 days on a consistent whole
food plant-based diet (WFPBD) full of fresh fruits, raw vegetables, nuts, seeds, and sprouts.
|
|
Keywords:Type-1 diabetes, Plant- based diet, Lifestyle medicine, Disease reversal, Nutrition
|
|
|
|
Introduction
|
|
| Diabetes is one of the most common metabolic disorders
that is associated with many life-threatening complications.
Diabetes is mainly of two types: type-2 diabetes (T2D) and
type-1 diabetes (T1D). T2D is the most common type of
diabetes worldwide. In T2D, impaired receptors do not
respond to insulin, eventually leading to insulin resistance
while in T1D, there is a deficiency of insulin produced in the
pancreas. It is caused by pancreatic dysfunction due to
autoimmune reaction in the body leading to the destruction
of beta cells, eventually leading to insulin deficiency. The
exact cause of T1D is a mystery. However, certain studies
demonstrate the mechanism by which A1 beta casein from
cow milk can lead to T1D1-7. Growing evidence shows the
association of the rise in vaccination doses and the rise in
T1D around the world8-11. Diet and lifestyle modification can
play a pivotal role in reversal of T1D and T2D by restoring
the glucose levels to non-diabetic range, thus either reducing
or eliminating the requirement of medicine/insulin.
|
|
|
Patient information
|
|
|
We present a case of a thirteen-year-old girl, weighing 28.5
kgs, who was diagnosed with T1D in Punjab, India in 2019.
Before diagnosis, she complained of frequent urination,
increased thirst, excessive fatigue, and weight loss. There
were extreme fluctuations in blood glucose levels. She was
injecting a total of about 25 units of insulin daily to maintain
her blood glucose readings. The patient approached the
author to assist her in dietary modification.
|
|
|
Therapeutic intervention
|
|
|
The patient agreed to follow a customised whole food plant�based diet (WFPBD) for an intervention period of 150 days.
This diet was divided into breakfast, lunch, and dinner.
Breakfast included three different types of fruits which
weighed 1% to 1.5% of body weight (in kilograms). In this
case it was between 280 and 420 grams of fruit for breakfast.
Lunch included three different types of raw vegetables
which weighed 0.5% to 1% of body weight along with a
customised vegan meal recipe. In this case it was 140 to 280
grams of raw vegetables followed by a customised vegan
meal recipe. Dinner was calculated the same way as lunch.
The patient’s preference for the cooked meal was
chappathies with vegetables and pulses. In addition to this,
soaked nuts and sprouts were also a part of the dietary
programme and the quantity of these was equal to 0.1% of
body weight. In this case it was about 28 grams each.
Packed, processed, fried, and refined foods were strictly
removed from her diet as they are an identified risk factor in
metabolic disorders12-17. Animal food and dairy products
were removed from the diet as these have been shown to
cause a negative effect on diabetics1-7. Blood glucose
readings were regularly monitored and necessary changes in
the diet schedule were made as and when required.
|
|
|
|
Follow up
|
|
|
The parents were also in touch with the concerned medical
doctor for assistance in adjustment of insulin dosage.
|
|
|
Results
|
|
|
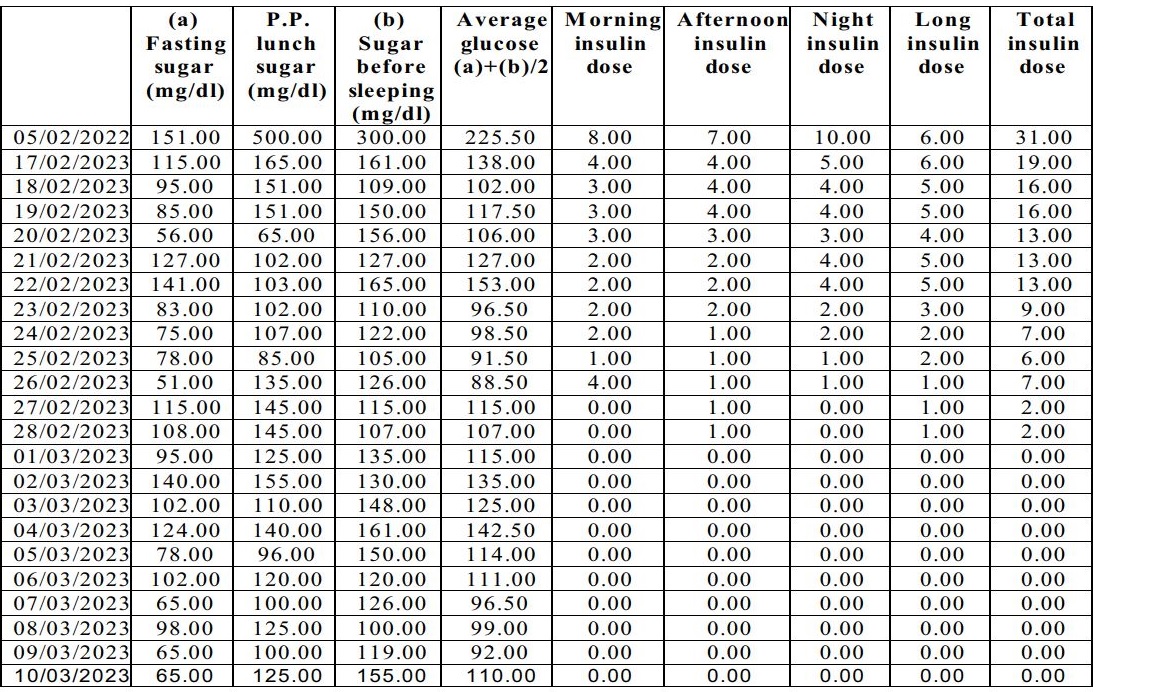
The table represents the daily glucose monitoring data of the
patient from 17.02.2023 to 10.03.2023. The patient
managed a fasting blood sugar (FBS) of 151 mg/dl and
average glucose (AG) of 225.50 mg/dl with 31 units of
insulin on 05.02.2022 before starting the dietary modification programme. The patient started the WFPBD
programme religiously from 17.02.2023 which consistently
regulated her blood sugar levels. On 17.02.2023 she took a
total of 13 units of fast-acting insulin and 6 units of long�acting insulin and her FBS was 115 mg/dl, PPG was 165
mg/dl, and AG was 161 mg/dl. With each passing day on
WFPBD her requirements to administer insulin reduced
consistently. On 27.02.2023 she did not inject insulin with
breakfast and dinner and maintained normal blood glucose
readings. Finally, she was able to eliminate her requirement
of injecting insulin entirely on 01.03.2023. Her FBS was 95
mg/dl, post prandial glucose (PPG) was 125 mg/dl, and AG
was 135 mg/dl on 01.03.2023. She did not require insulin
injections after 01.03.2023 to regulate her blood glucose
levels as monitored till 31.07.2023.
|
|
|
|
|
|
|
|

The graph represents the gradual reduction in the daily insulin requirements of the patient. On 17.02.2023 she took 13 units of fast�acting insulin and 6 units of long-acting insulin. With each passing day on WFPBD her insulin requirements reduced consistently, and
she was able to eliminate her requirement of insulin injections on 01.03.2023.
|
|
|
|
|
Outcomes
|
|
|
Before intervention: : On 05.02.2023, her fasting blood
glucose (FBG) was 151 mg/dl, average PPG was 400
mg/dl, and she took 31 units of insulin to manage her
blood glucose readings.
|
|
After intervention: : She started following the prescribed
whole food plant-based diet from 17.02.2023. Her
average FBG readings were 93 mg/dl and average PPG
readings were 134 mg/dl between 01.03.2023 and
10.03.2023. Her average FBG readings were 79 mg/dl
and average PPG readings were 165 mg/dl between
03.07.2023 and 12.07.2023. She is maintaining a non�diabetic glucose range by following the diet programme
consistently. Her blood glucose readings were regularly
monitored till 31.07.2023.
|
|
|
Discussion
|
|
|
There is a continuous rise in cases of T1D around the world.
The potential cause may be genetics triggered by a wrong
choice of food habits, including consumption of processed
milk of A1 cows, and increasing number of doses in the
vaccine schedule. Dietary modification can provide good
support in remission of T1D and T2D without causing any
side effects. In this case study, we present a comprehensive
analysis by stating the difference of blood glucose changes
before and after the dietary intervention in a T1D patient.
She was diagnosed with T1D in 2019 and has been taking
insulin injections since then to manage her blood glucose
readings. However, she was able to eliminate insulin
dependency within 14 days of adopting a whole food plant�based diet full of fresh fruits, raw vegetables, nuts, seeds,
and sprouts. Her glucose levels are also in the non-diabetic
range as followed up till 31.07.2023 without insulin
administration.
|
|
|
Conclusion
|
|
|
The effect of dietary modification on type-1 diabetics should
be prospectively evaluated in a large multicentre
randomised nutrition intervention trial. Nutritional
intervention can be a potential tool for remission of type-1
diabetes in the future of clinical practice.
|
|
|
References
|
|
1. Gerstein HC. Cow's milk exposure and type I diabetes
mellitus. A critical overview of the clinical literature.
Diabetes Care. 1994 Jan; 17(1):13-9.
2. Dahl-Jørgensen K, Joner G, Hanssen KF. Relationship
between cows' milk consumption and incidence of IDDM in
childhood. Diabetes Care. 1991 Nov; 14(11); 1081-3.
3. Virtanen SM, Räsänen L, Aro A, et al. Infant feeding in
Finnish children less than 7 year of age with newly
diagnosed IDDM. Childhood Diabetes in Finland Study
Group. Diabetes Care. 1991 May; 14(5):415-7.
4. Perez-Bravo F, Carrasco E, et al. Genetic predisposition
and environmental factors leading to the development of
insulin-dependent diabetes mellitus in Chilean children.
Journal of Molecular Medicine (Berl).1996 Feb; 74(2):105-
9.
5. Monetini L, Cavallo MG, et al; IMDIAB Group. Bovine
beta-casein antibodies in breast- and bottle-fed infants: their
relevance in Type 1 diabetes. Diabetes/ Metabolism Research and Reviews. 2001 Jan-Feb; 17(1):51-4.
6. Kimpimäki T, Erkkola M, et al. Short-term exclusive
breastfeeding predisposes young children with increased
genetic risk of Type I diabetes to progressive beta-cell
autoimmunity. Diabetologia. 2001 Jan; 44(1):63-9.
7. Kostraba JN, Cruickshanks KJ, et al. Early exposure to
cow's milk and solid foods in infancy, genetic
predisposition, and risk of IDDM. Diabetes. 1993 Feb;
42(2):288-95. PMID: 8425665.
8. Classen, John Barthelow. Review of vaccine induced
immune overload and the resulting epidemics of type 1
diabetes and metabolic syndrome, emphasis on explaining
on the recent accelerations in the risk of prediabetes and
other immune mediated diseases. Journal of Molecular and
Genetic Medicine 2014 (2014): 1-4.
9. Wahlberg J, Fredriksson J, et al; Abis Study Group.
Vaccinations may induce diabetes-related autoantibodies in
one-year-old children. Annals of the New York Academy of Sciences; 2003 Nov; 1005:404-8.
10. Classen, John Barthelow. Risk of vaccine induced
diabetes in children with a family history of type 1 diabetes.
The Open Pediatric Medicine Journal 2008. 2. 7-10.
10.2174/1874309900802010007.
11. Classen JB, Classen DC. Vaccines and the risk of
insulin-dependent diabetes (IDDM): potential mechanism
of action. Medical Hypotheses. 2001 Nov; 57(5):532-8.
12. Levy RB, Rauber F, et al. Ultra-processed food
consumption and type 2 diabetes incidence: A prospective
cohort study. Clinical Nutrition. 2021 May; 40(5):3608-
3614.
13. Lane MM, Davis JA, et al. Ultraprocessed food and
chronic noncommunicable diseases: A systematic review
and meta-analysis of 43 observational studies. Obesity
Reviews. 2021 Mar; 22(3):e13146.
14. Mendonça RD, Pimenta AM, et al. Ultraprocessed food
consumption and risk of overweight and obesity: the
University of Navarra follow-up (SUN) cohort study.
American Journal of Clinical Nutrition. 2016 Nov;
104(5):1433-1440.
15. Delpino FM, Figueiredo LM, Bielemann RM, et al.
Ultra-processed food and risk of type 2 diabetes: A
systematic review and meta-analysis of longitudinal studies.
International Journal of Epidemiology; 2022 Aug 10;
51(4):1120-1141.
16. Almarshad MI, Algonaiman R, Alharbi HF, et al.
Relationship between ultra-processed food consumption
and risk of diabetes mellitus: Amini-review. Nutrients. 2022
Jun 7; 14(12):2366.
17. Esselstyn, Jr., C. B. (2019). Is Oil Healthy? International
Journal of Disease Reversal and Prevention, 1(1), 3 pp.
|
|
|
|
|
|
|
Dr. Kamalpreet Singh
A3 Sukh Sehaj Enclave, Anandpur Sahib
Punjab, India - 140118
Ph: +919718422691
Email: coolkamal1997@gmail.com
|
|
|
|
|
|
|
|
|
|
|
|
|
|
New Updates
|
|
|
|
|
|
|
|
|
|
|